QI initiative improves the safer administration of medicines in a Birmingham care home
In March 2021, staff at Marian House Nursing Home embarked on a Quality Improvement (QI) initiative to improve the safer administration of medicines for people living in the home. Marian House Nursing Home is a 42 bedded care home in the Sutton Coldfield area of Birmingham that provides nursing and residential care, led by manager Jo Stinton.
The QI initiative was part of a National Medicines Safety Improvement Programme (MedSIP) commissioned by NHS England and Improvement (NHSE/I) which aims to improve the safer administration of medicines in care homes. The West Midlands Patient Safety Collaborative (WMPSC), who are leading this work in the West Midlands region, invited expressions of interest from care homes in the region to be part of this pioneering improvement work.
Jo Stinton, Manager at Marian House was first introduced to QI tools and techniques back in 2019 when she completed a Leadership and Development programme with My Home Life. My Home Life had delivered very successful development programmes for care home managers for many years, however the programme was enhanced by the addition of a QI module (sponsored by the WMAHSN) and this proved to be invaluable to the effectiveness and outcomes of the leadership programme. Read more about Marion House’s previous success here.
Marian House have always been keen to improve the quality of care for residents and have a track record of implementing QI projects successfully. Staff identified an interest in undertaking a QI project to improve safer administration of medicines for residents, by reducing the number of avoidable interruptions to medicine rounds. This is important because medicine rounds are a safety critical activity and distractions caused by interruptions may result in error, which has potential to cause harm related incidents.
The Care Home Use of Medicines Study (CHUMS report) published in 2009 outlined the prevalence, causes and potential harm of medication errors in 55 care homes for older people. The report revealed an unacceptable level of medication errors relating to older people in care homes. The study showed that care home residents take an average of eight different medicines every day. On any one day, seven out of ten residents experience mistakes with their medications. These errors range from doses being missed or given incorrectly, to the wrong drugs being given out. In some cases, these errors have the potential to cause very serious harm. Distractions during medicine rounds are one potential source of error.
Staff were supported by Caroline Maries-Tillott the QI lead at the WMPSC to use the IHI Model for Improvement to guide their improvement project. Staff started the project by collecting baseline data about the number of interruptions to medicine rounds. Staff audited the number of interruptions to medicine round over a period of 3 weeks- including the reason for the interruption and who the interruption was by. This data was then presented back to staff and staff agreed a SMART aim for the project and improvement ideas were generated.
*All Model for Improvement references are taken from: Langley, G, Moden, R et al. 2009. The Improvement Guide. A Practical Approach to Enhancing Organizational Performance. 2nd Ed. San Francisco: Jossey-Bass.
Marian House Care Home AIM
The baseline data showed that medicine rounds were interrupted frequently, with the morning medicine round being the most frequently interrupted. Baseline data showed that the morning medicine round was interrupted on average of 3 times.
Using the baseline data staff agreed the following SMART aim for their improvement project:
To reduce the number of avoidable interruptions to medicine rounds by 1/3rd over the next month (from an average of 3 interruptions in the most frequently interrupted medicine morning round to 2 per morning round )
A (COVID safe) staff meeting was held. All staff regardless of role were invited.

This is important in any QI project to ensure that there is collective aim setting and staff understand their contribution to the collective aim. Staff included Senior Carers and Carers; Domestics; Nurses; Activity Co-Ordinator, Laundry Staff; Cooks and Administrative Staff.
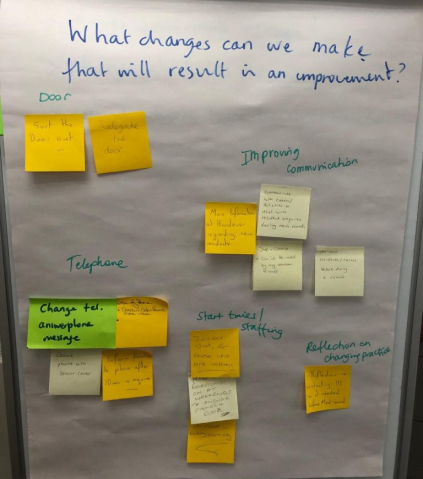
Staff identified a number of potential improvement ideas to test out, to see if they would be successful in achieving their aim of reducing interruptions to medicine rounds over the next month.
The Improvement Ideas
The ideas fell into 3 themes:
- Culture change, change of practice and reminder
- Relaunch of procedure
- Protocol relating to other communication methods
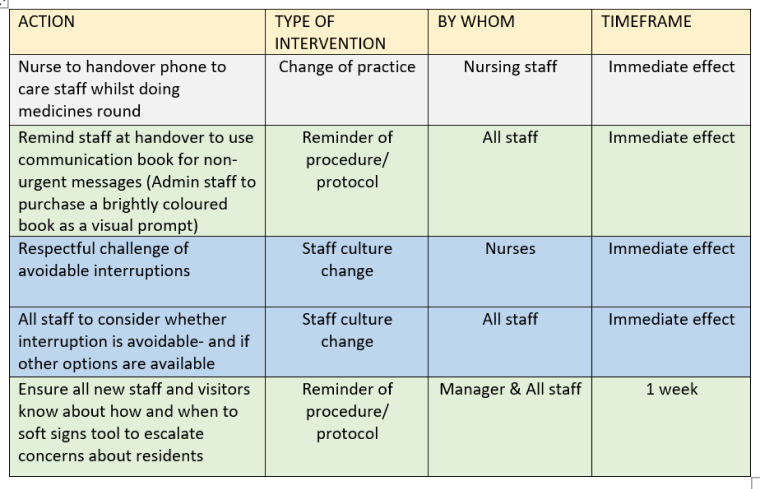
The table below shows a number of interventions identified by staff for testing. Staff continued to audit the number of interruptions to medicine rounds so that they could track whether or not the interventions were driving a reduction in the number of interruptions.
Impact on interruptions to medicine rounds
It was recognised at the onset that not all interruptions are avoidable, particularly if there is a safety issue that requires urgent action. Interruptions by residents are sometimes also unavoidable given the high number of people with dementia. However, the data showed significant and sustained reductions were noted in ALL medicine rounds following implementation of the improvement interventions!
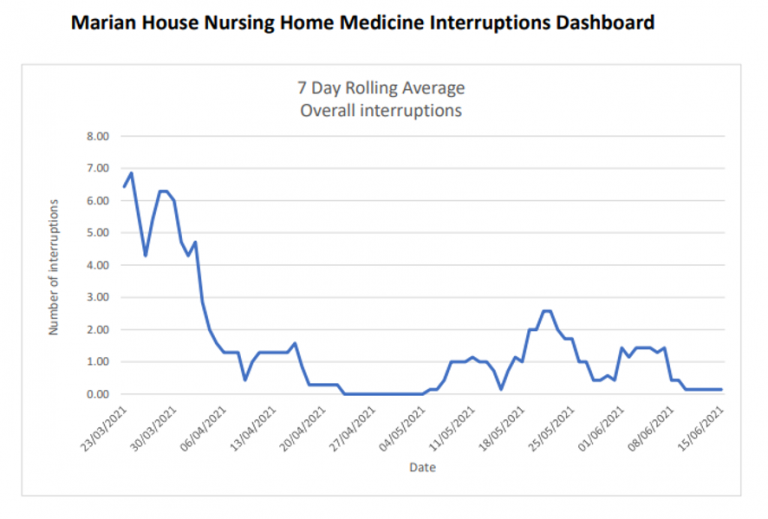
Indeed, results show that the original care home AIM to reduce the number of avoidable interruptions to the morning medicine round by 1/3rd over the next month was not only achieved but surpassed.
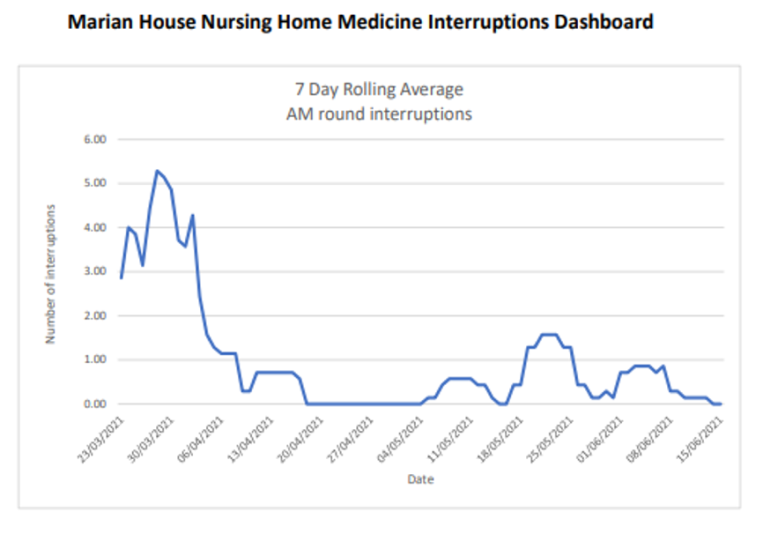
An important part of any QI project is to track progress and share the results with staff. This engages and motivates staff to discuss what is working well and what interventions may need to be adapted. In addition to staff meetings where results have been shared and celebrated, the manager has also developed posters to thank staff for their efforts and celebrate their achievements.
“The improvements achieved at Marian House Nursing home represent a significant culture shift towards safer medicines administration for the residents that they care for. The methodology and results from this improvement project have been shared with other Patient Safety Collaboratives across the country that are also engaged with similar medicines related improvement work. It is anticipated that similar improvement will be realised in care homes across the country, supporting the ambition to improve the safer administration of medicines for vulnerable residents in care homes.”
Article by Caroline Maries-Tillott
Quality Improvement Lead WMAHSN